As of 2020, approximately 5.8 million Americans suffer from Alzheimer’s disease, but recent groundbreaking research may provide hope to better understand and potentially prevent this devastating condition. The study led by researchers at New York Medical College (NYMC) and Eastern Virginia Medical School and published in Nature Communications Biology has unveiled a crucial link between diet, inflammation and Alzheimer’s disease, shedding light on potential pathways for intervention.
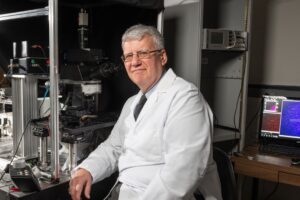
“Inflammation in the brain is a critical force in the generation and progression of Alzheimer’s disease. The Western diet, which is high in fat and cholesterol, can further increase this inflammation. We found that preventing a certain protein from activating genes that cause inflammation can protect the brain from the effects of the Western diet. This discovery offers the incredibly exciting prospect of new treatments that may slow or even stop Alzheimer’s disease in its tracks,” said Patric Stanton, Ph.D., professor of cell biology and anatomy and of neurology at NYMC.
According to the study, which was supported by a grant from the National Institutes of Health, there is a well-known association between diabetes, metabolic syndrome and an increased risk of cognitive dysfunction and Alzheimer’s disease. Diabetes, in particular, can lead to atherosclerosis and vascular inflammation, which are thought to trigger Alzheimer’s disease in susceptible individuals. The Western diet is a major cause of metabolic issues.
“A better understanding of the causes of early brain dysfunction could lead to earlier identification and treatments to improve care and outcomes for patients,” said Jerry Nadler, M.D., former dean of the School of Medicine and adjunct professor of pharmacology at NYMC and associate chief of staff for research and development at the Northern California Veterans Health System.
The research focused on the transcription factor, STAT 4, which plays a significant role in inflammation activation in the body. When STAT4 was intact, prolonged feeding with a Western diet, led to a diabetes-like metabolic syndrome characterized by impaired sensitivity to glucose and insulin, indicating early diabetes. However, genetically modified mice lacking STAT4 in their brains were fully protected when fed the same diet and showed less brain activation of a range of inflammatory genes.
One of the most exciting findings from the study involved its impact on memory. While long-term, synaptic activity-dependent plasticity, a process underlying memory formation, was found to be impaired by the Western diet, this damage was prevented when STAT4 was not present. “This suggests that early changes linked to Alzheimer’s disease can be prevented even on the high-fat diet through targeted deletion of STAT4,” said Dr. Stanton.